Take breaks when binge-watching TV to avoid blood clots, say scientists. The warning comes as a study reports that watching TV for four hours a day or more is associated with a 35 per cent higher risk of blood clots compared with less than 2.5 hours. The University of Bristol research is published today in the European Journal of Preventive Cardiology, a journal of the ESC.
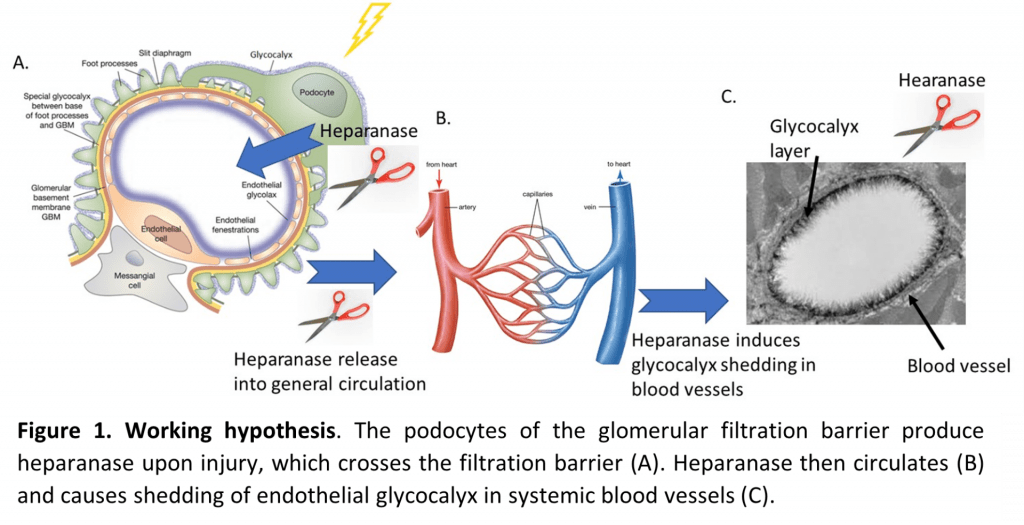
The study examined the association between TV viewing and venous thromboembolism (VTE). VTE includes pulmonary embolism (blood clot in the lungs) and deep vein thrombosis (blood clot in a deep vein, usually the legs, which can travel to the lungs and cause pulmonary embolism).
To conduct the study, the University of Bristol researchers conducted a systematic review to collect the available published evidence on the topic and then combined the results using a process called meta-analysis.
Lead author, Dr Setor Kunutsor from the University’s Bristol Medical School explained:
“Combining multiple studies in a meta-analysis provides a larger sample and makes the results more precise and reliable than the findings of an individual study.”
The analysis included three studies with a total of 131,421 participants aged 40 years and older without pre-existing VTE. The amount of time spent watching TV was assessed by questionnaire and participants were categorised as prolonged viewers (watching TV at least four hours per day) and never/seldom viewers (watching TV less than 2.5 hours per day).
The average duration of follow-up in the three studies ranged from 5.1 to 19.8 years. During this period, 964 participants developed VTE. The researchers analysed the relative risk of developing VTE in prolonged versus never/seldom TV watchers. They found that prolonged viewers were 1.35 times more likely to develop VTE compared to never/seldom viewers.
The association was independent of age, sex, body mass index (BMI) and physical activity. Dr Kunutsor said:
“All three studies adjusted for these factors since they are strongly related to the risk of VTE; for instance, older age, higher BMI and physical inactivity are linked with an increased risk of VTE.
“The findings indicate that regardless of physical activity, your BMI, how old you are and your gender, watching many hours of television is a risky activity with regards to developing blood clots.
“Our study findings also suggested that being physically active does not eliminate the increased risk of blood clots associated with prolonged TV watching,” said lead author Dr Kunutsor. “If you are going to binge on TV you need to take breaks. You can stand and stretch every 30 minutes or use a stationary bike. And avoid combining television with unhealthy snacking.”
Dr Kunutsor noted that the findings are based on observational studies and do not prove that extended TV watching causes blood clots.
Regarding the possible reasons for the observed relationship, he said:
“Prolonged TV viewing involves immobilisation which is a risk factor for VTE. This is why people are encouraged to move around after surgery or during a long-haul flight. In addition, when you sit in a cramped position for long periods, blood pools in your extremities rather than circulating and this can cause blood clots. Finally, binge-watchers tend to eat unhealthy snacks which may lead to obesity and high blood pressure which both raise the likelihood of blood clots.”
Dr Kunutsor concluded:
“Our results suggest that we should limit the time we spend in front of the television. Long periods of TV watching should be interspersed with movement to keep the circulation going. Generally speaking, if you sit a lot in your daily life – for example your work involves sitting for hours at a computer – be sure to get up and move around from time to time.”
Read the paper
Television viewing and venous thrombo-embolism: a systematic review and meta-analysis in the European Journal of Preventive Cardiology by Setor Kunutsor, Richard Dey and Jari Laukkanen.
Further information
Authors’ note:
The findings are based on observational studies, so they do not prove cause and effect.
These findings are based on the results of only three studies. More studies are needed to confirm or refute the findings.