Two new grants will further BHI research into progeria and pulmonary hypertension:
MRC: Gene-inspired therapy to rescue cardiovascular disease in progeria: awarded to Professor Paolo Maddedu
Hutchinson-Gilford progeria syndrome (HGPS), characterised by a rapidly ageing appearance, is a rare disease caused by an abnormal gene and related protein. Because there is no effective cure, children with HGPS will, on average, die of cardiovascular disease at around 14 years old.
This project proposes a new treatment where a gene – found in people who live a long and healthy life – is transferred to rescue the premature cardiovascular senescence typical of HGPS patients.
Professor Paolo Madeddu’s team has discovered a beneficial variant of the BPIFB4 gene, and shown in animal models that transferring this gene reduces the suffering from a heart attack, diabetes and high blood pressure. Preliminary studies showed that the longevity BPIFB4 mutation can benefit some molecular mechanisms that are dysfunctional in children with HGPS.
Paolo says:
“We will determine the efficacy of BPIFB4 gene therapy in HGPS mice, looking at the treatment’s ability to preserve heart and blood vessel function. In addition, we will investigate the mechanisms underpinning this benefit, using human cells from HGPS patients. If results are positive, we will continue our research confirming the lack of toxicity, defining the best dose and timing of treatment for prolonged benefit and the advantage of adding BPIFB4 therapy to current drugs, in view of obtaining permission for a clinical study in patients.”
HRUK: Targeting pericytes for halting pulmonary hypertension in infants with CHD: awarded to Professor Paolo Madeddu, Professor Massimo Caputo and Dr Elisa Avolio
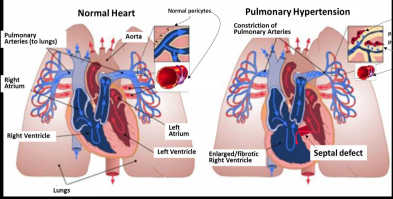
Some children are born with a ventricular septal defect: a hole in the wall between the two lower chambers of the heart, where blood can flow across the hole from the left side of the heart to the right. If the defect is not corrected in time, children are likely to develop pulmonary hypertension (high pressure in the blood circulation to the lung).
Surgical correction of the ventricular shunt usually allows the blood pressure in the lungs to return to normal levels. In some cases, however, the pressure may stay higher than normal after surgery.
At least five to 10 per cent of patients with congenital heart disease develop pulmonary arterial hypertension (PAH), which can lead to heart failure. The risk of developing pulmonary hypertension is higher for children living in poor countries and areas of social deprivation, because of the limited access to specialist centres where the cardiac defect can be recognised and corrected before complications arise.
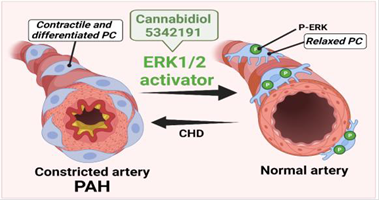
Recent research indicates pericytes – multi-functional cells embedded within the walls of capillaries – could be targeted for the treatment of PAH. Paolo says:
“Our research will investigate why pericytes from children with CHD constrict and block the pulmonary circulation. It will also test a new treatment to reduce the contraction of pulmonary pericytes and prevent pulmonary hypertension occurring.”